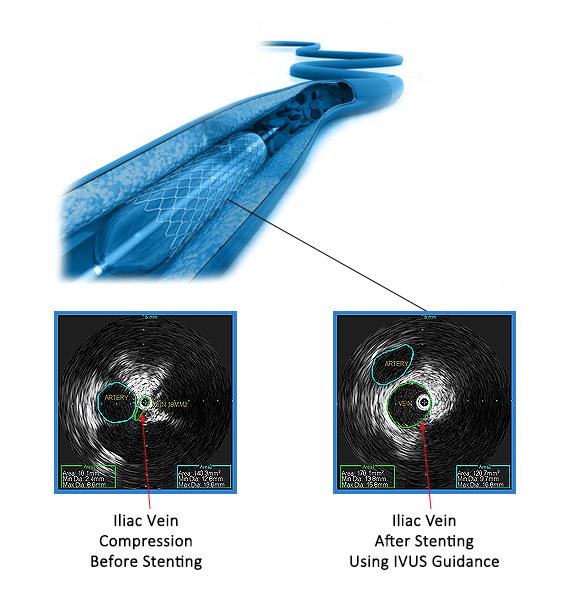
Iliac Vein Stenting
Iliac Vein Stenosis
Iliac vein stenosis (narrowing) or compression is a frequently under-diagnosed condition which may result in leg edema, discomfort, venous stasis skin changes varying from hyperpigmentation to ulcers. Many symptoms often seen in patients with venous insufficiency may actually be due to iliac vein stenosis or compression. In severe cases, patients may have pain with walking, so-called “venous claudication”.
Some patients present with an iliac deep vein thrombosis (DVT) which, after treatment, is typically due to compression of the left iliac vein by the overlying right iliac artery. This is known as “May-Thurner Syndrome”. However, many patients have a less sudden course due to areas of iliac vein stenosis from fibrosis (“scarring”) of the vein.
Diagnosis of Iliac Vein Stenosis
One of the reasons iliac vein stenosis / compression is underdiagnosed is that the condition is quite difficult to identify non-invasively. lliac vein stenosis is difficult to visualize with external ultrasound, CT scan or magnetic resonance imaging. The most reliable test requires placement of an intravascular ultrasound (“IVUS”) catheter into the iliac veins in the catheterization laboratory and measuring the cross-sectional area of the vein compared to normal values. The hemodynamic changes in veins are different from those in arteries. While arterial blockages are typically not treated unless more than 70% stenosis, venous obstruction is considered significant if more than 50%.
Treatment of Iliac Vein Stenosis
Highly specialized stents have been developed for treatment of iliac vein stenosis. These stents are designed for maximum flexibility as well as strength to resist compression. As with all stents, certain blood thinners are required for at least several months to prevent any clots from forming on or within the stents. Patients often experience remarkable improvement in their symptoms within days of the stent procedure.